Spine surgery has seen groundbreaking transformations in recent years, offering improved outcomes for patients with complex spinal conditions. As medical technology advances, surgeons now have access to innovative techniques and technologies that promise more precise, less invasive, and more effective treatments.
This article will focus on improvements in areas such as spinal stenosis surgery, treatments for spondylolisthesis, and other conditions that can severely impact a person’s quality of life.
Understanding the Challenges of Spinal Conditions
Spinal stenosis and spondylolisthesis are debilitating conditions that can significantly impact a patient’s quality of life.
- Spinal stenosis occurs when the spinal canal narrows, putting pressure on the nerves and causing pain, numbness, and weakness.
- Spondylolisthesis involves one vertebra slipping over another, leading to instability, pain, and potential nerve compression.
Traditionally, these conditions required highly invasive surgical interventions with lengthy recovery times.
How Spinal Conditions Impact Quality of Life
Spinal conditions can disrupt an individual’s daily life, transforming simple activities into challenging ordeals. Chronic pain significantly impacts a person’s daily life, affecting work productivity and personal relationships. Patients often experience a cascading impact on their physical and mental well-being.
Movement becomes restricted and painful, limiting mobility and independence. Activities once taken for granted—walking, sitting for extended periods, or playing with children—suddenly become daunting tasks. The constant discomfort can lead to decreased physical activity and contribute to muscle weakness, weight gain, and further health complications.
There are also psychological consequences caused by persistent pain and reduced mobility, which frequently trigger depression, anxiety, and social isolation. Many patients report feeling frustrated, helpless, and disconnected from their previous lifestyle. The economic burden of medical treatments, potential job limitations, and ongoing healthcare expenses compound the emotional strain.
Minimally Invasive Surgical Techniques:
Endoscopic Spine Surgery
One of the most significant breakthroughs in spine surgery is the development of endoscopic techniques. Unlike traditional open surgeries that require large incisions and extensive muscle disruption, endoscopic spine surgery uses tiny cameras and specialized instruments inserted through small cuts, often less than one inch.
This approach offers numerous advantages, such as:
- Reduced muscle and tissue damage
- Faster recovery times
- Decreased post-operative pain
- Lower risk of infection
- Minimal scarring

For patients with spinal stenosis, endoscopic decompression makes it easier for surgeons to remove bone spurs and ligament tissue with improved precision, relieving nerve pressure while minimizing surgical trauma.
Robotic-Assisted Spine Surgery
Robotic technology has become a key part of spine surgery, providing surgeons with enhanced precision and control. These advanced systems use pre-operative imaging to create detailed 3D models, allowing for extremely accurate implant placement and customized surgical plans. As a result, patients are subjected to less radiation exposure and benefit from improved surgical outcomes as there is a minimized risk of human error
Spondylolisthesis patients can greatly benefit from robotic-assisted procedures, which help surgeons achieve high-accuracy vertebral alignment and stabilization.
Advanced Imaging and Navigation Technologies
Modern spine surgeries now incorporate sophisticated navigation systems that provide real-time, high-resolution guidance during procedures.
CT scans and advanced imaging allow surgeons to:
- Visualize spinal structures
- Make real-time adjustments
- Ensure precise instrument placement
- Minimize risks associated with complex surgeries
Biological and Regenerative Approaches
Stem Cell and Growth Factor Therapies
Emerging regenerative medicine techniques are revolutionizing spine surgery recovery. Stem cell treatments and growth factor therapies can accelerate healing, reduce inflammation, boost tissue regeneration, and potentially reduce the need for extensive surgical interventions. For patients with degenerative spinal conditions, these therapies offer hope for more comprehensive healing and potentially slower disease progression.
Artificial Disc Replacement: Beyond Fusion
Traditional spinal fusion surgeries limited patient mobility and increased stress on adjacent spine segments. Artificial disc replacement represents a significant advancement by preserving natural spine movement, reducing the risk of adjacent segment disease, and enabling faster recovery. Particularly for spondylolisthesis, these technological implants can provide stability without eliminating spinal flexibility.
Machine Learning and Predictive Analytics
Artificial intelligence (AI) and machine learning (ML) are making significant inroads into spine surgery planning and outcomes prediction. As ML algorithms can analyze vast patient datasets, they are more effective at predicting surgical risks and creating customized treatment plans to increase success rates. These algorithms also improve long-term patient outcomes by identifying potential complications before they occur.
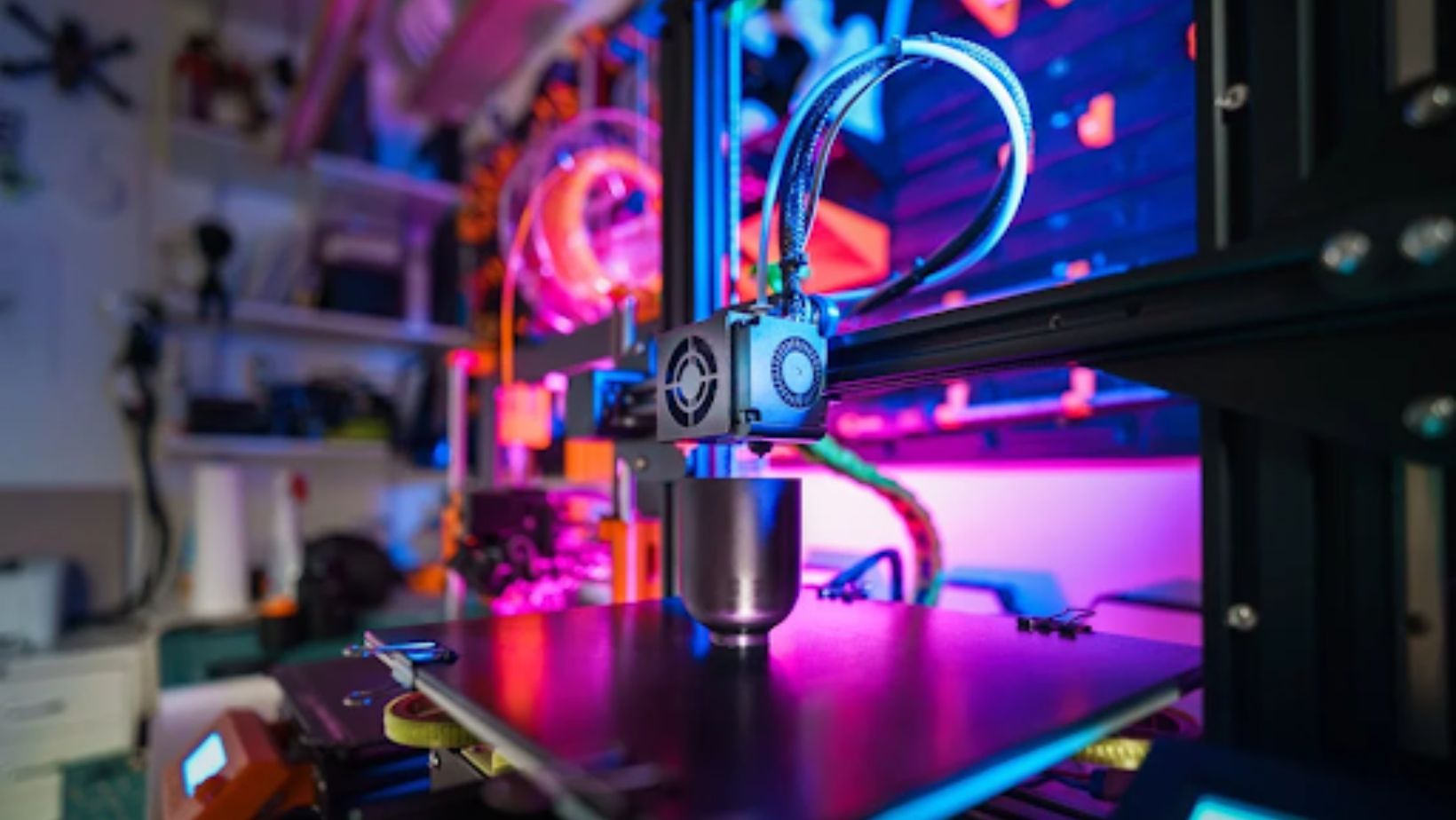
Personalized 3D-Printed Implants
3D printing technology now allows for completely customized spinal implants tailored to individual patient anatomy.
These patient-specific solutions offer:
- Perfect geometric matching
- Improved implant integration
- Reduced risk of complications
- Enhanced structural compatibility
Challenges and Future Directions
Despite recent innovations, challenges remain. These include cost, accessibility, and the need for specialized training. These factors continue to impact widespread adoption. However, the trajectory of spine surgery is clear and is becoming increasingly more precise and less invasive, helping to create more personalized treatments.
Mechanical Spinal Devices Vs. Spinal Fusion
Mechanical spinal devices are a significant advancement over traditional spinal fusion techniques, offering patients a more dynamic and less damaging approach to treating complex spinal conditions. Unlike spinal fusion, which permanently immobilizes a segment of the spine by connecting vertebrae, mechanical devices are designed to maintain and potentially restore natural spinal movement while providing the necessary stability.
Traditional fusion surgery eliminates motion at the affected spinal segment, which can lead to increased stress on adjacent vertebral levels. This is known as adjacent segment disease and can cause accelerated degeneration of the spine segments above and below the fusion site.
In contrast, mechanical devices like artificial disc replacements allow for continued natural movement, distributing mechanical stress more evenly across the spine and potentially reducing the long-term risk of additional spinal degeneration.
Conclusion
The landscape of spine surgery is evolving at an unprecedented pace. For patients with conditions like spinal stenosis and spondylolisthesis, these innovations offer more than just treatment—they provide hope for improved quality of life, reduced pain, and restored mobility.
As technology continues to advance, we can expect even more groundbreaking developments that will transform how we approach spinal health. The future of spine surgery is not just about treating conditions but about providing comprehensive, patient-centered solutions that address both immediate medical needs and long-term well-being.
Thank you for reading. We hope this article has provided some interesting insights into modern spinal surgery innovations.

